There are neurophysiological effects from witnessing and experiencing events that violate systems embedded within us. These systems are designed to keep us safe and make us care deeply for others. Past events interact with our socio-neurobiology, and can get suppressed, which leads to internal distress and maladaptive strategies that negatively impact mental health and wellbeing.
Trauma can lead people’s nervous system to shut off access to certain affective states. Unfortunately, this often shuts off access to circuits needed for releasing sorrow, guilt, shame and for re-connecting with joy.
We live in a world immersed in unhealed trauma. As a species, we are only beginning to learn how to heal from past events and consciously regulate ourselves - on our own and with others.
We need raw, real conversations about the unhealed wounds we witness in ourselves and in our parents, families, and social circles. In research I contributed to last year for the University of Calgary, we focused on how to engage communities and families in strengths-based approaches to trauma healing and recovery. Healing comes from social connectedness and safe spaces for people to share their stories and their healing journey.
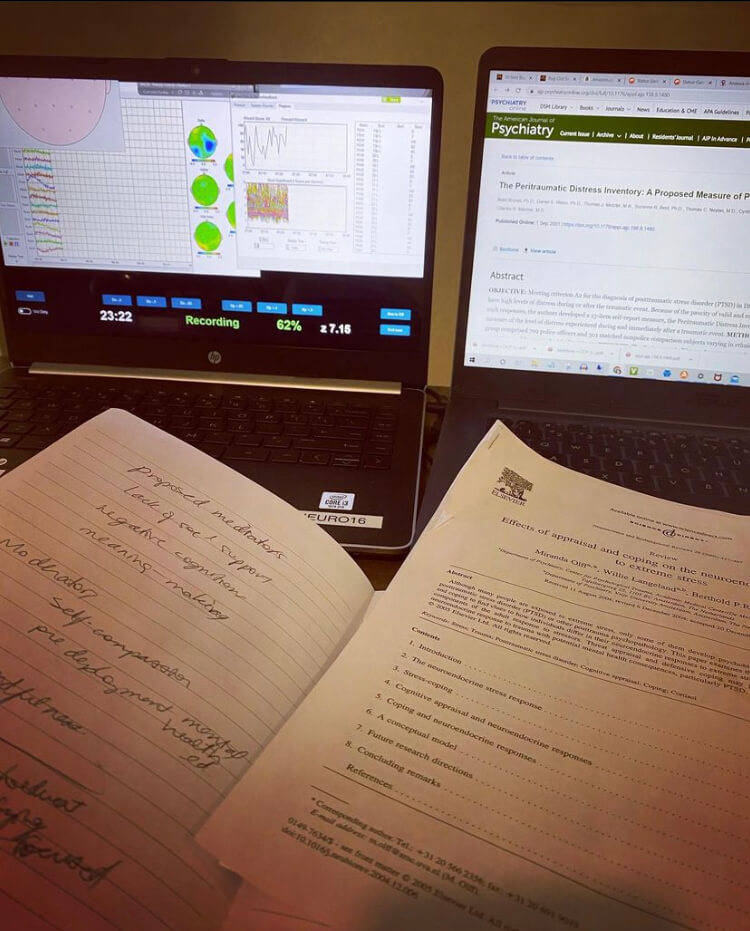
We need to arm ourselves with, model and teach others new ways to navigate emotional and mental distress, and how to adaptively interpret the physiological sensations from the brain-body as it responds to stimuli. The more we can understand how all this works from a bio-mechanical perspective, the more we can create measurements to help prevent and treat post-trauma physiology and widen the range of healing modalities to include community and family-based interventions, body, breath and movement therapies, narrative and story-telling, somatic experiencing and neurotechnology treatments (like MeRT and neurofeedback), as well as therapies that increase cognitive flexibility and meaning-making (such as those found in Acceptance and Commitment Therapy, Cognitive and Dialectical Behavior Therapy, and Adaptive Disclosure).
As cliché as it sounds, we also need more love and compassion for ourselves and others. Compassion is a state of openness that requires flexible thinking and holding complex perspectives. Without it, we stay within the confines of self-protective mechanisms of our brain-body system.
Complex and emotionally challenging times… we need as many of us coming together to understand and collaborate to learn how to heal from the massive effects trauma has on our brain-body system, and on us collectively as a species.
To all of you who are focused on helping break the cycles of unhealed wounds, the world thanks you 🙂
With Love from Me to You
xoxo Stefanie
Warriors Heart Foundation is contributing to a wide range of treatment modalities and support (such as those listed above). I’ll be interviewing them for an upcoming episode of the Mindset Neuroscience Podcast
References
Outcomes of participation in the REACH multifamily group program for veterans with PTSD and their families. Fischer, E. P., Sherman, M. D., Han, X., & Owen, R. R., Jr. (2013).
Cognitive-behavioral conjoint therapy for PTSD improves various PTSD symptoms and trauma-related cognitions: Results from a randomized controlled trial, Macdonald, A., Pukay-Martin, N. D., Wagner, A. C., Fredman, S. J., Monson, C. M. (2015).
Participants' perceived benefits of family intervention following a first episode of psychosis: a qualitative study, Nilsen, L., Frich, J. C., Friis, S., Norheim, I., & Røssberg, J., I. (2014).
Stigma, Pluralistic Ignorance, and Attitudes Toward Seeking Mental Health Services Among Police Officers, Karaffa, K. M., & Koch, J. M. (2015).
Functional disconnection and reconnection: an alternative strategy to stoicism in public safety personnel, McElheran, M. & Stelnicki, A. M. (2021)
Impact of Canadian Armed Forces Veterans’ Mental Health Problems on the Family During the Military to Civilian Transition, Cramm, H., Norris, D., Schwartz, K., Tam-Seto, L., Williams, A., & Mahar, A. (2020).
Review of Mental Health Support for Veteran Families: A Demographic Survey Using the 2016 Life After Service Survey (LASS), Schwartz, K. (2017).
Family members of Veterans with mental health problems: Seeking, finding, and accessing informal and formal supports during the military-to-civilian transition, Schwartz, K., Norris, D., Cramm, H., Tam-Seto, L., & Mahar, A. (2021).
I also have a few articles on trauma healing and moral injury:
Psychic Trauma and Annihilation Anxieties
Season 2 Episode 12: Moral Injury, Forgiveness and Cognitive Flexibility
Moral Injury and Post-Traumatic Healing

Grateful for our mammalian, oxytocinergic heritage that allows us to experience safe human connection and closeness.

Thankful that a few of my closest friends have little ones for me to hold and play with 🙂 We need them as much as they need us.
I'll be posting some content soon about concepts from childhood development research and how we optimize learning, exploration and self-regulation in kids.
#resilience #neuroscience #cometogether #familyunit #powerpartnerships #team #mission #purpose #endurance #warriorsheart #genx #mentalhealth #moralinjury #traumahealing #unhealedwounds #invisiblewounds #awakening #unraveling #crisis #passingdownwisdom #futuregenerations